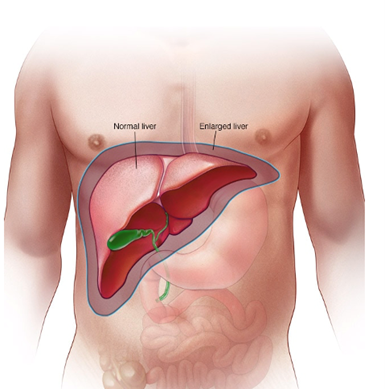
 The liver acts as the gatekeeper of the body in that it filters, stores, protects, and breaks down substances among other things. When the liver cannot work properly, there can be significant health issues. It is found in the right upper quadrant of the abdomen, just below the diaphragm. It consists mainly of two lobes that can be divided into eight segments. Within these segments are called lobules, which are the functional units of the liver. Lobules contain hepatocytes—also referred to as liver cells! These hepatocytes do much of the functioning in the liver.
The liver acts as the gatekeeper of the body in that it filters, stores, protects, and breaks down substances among other things. When the liver cannot work properly, there can be significant health issues. It is found in the right upper quadrant of the abdomen, just below the diaphragm. It consists mainly of two lobes that can be divided into eight segments. Within these segments are called lobules, which are the functional units of the liver. Lobules contain hepatocytes—also referred to as liver cells! These hepatocytes do much of the functioning in the liver.
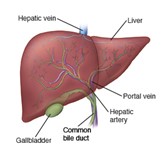 The liver receives blood supply from two different sources, one being the hepatic artery, which comprises of blood that is rich in oxygen and feeds all the cells of the liver oxygen. The second source is the hepatic portal vein, which is very poor in oxygen, yet rich in nutrients. The hepatic portal vein derives from the digestive system, breaks down food, and transports the necessary nutrients to the liver.
The liver receives blood supply from two different sources, one being the hepatic artery, which comprises of blood that is rich in oxygen and feeds all the cells of the liver oxygen. The second source is the hepatic portal vein, which is very poor in oxygen, yet rich in nutrients. The hepatic portal vein derives from the digestive system, breaks down food, and transports the necessary nutrients to the liver.
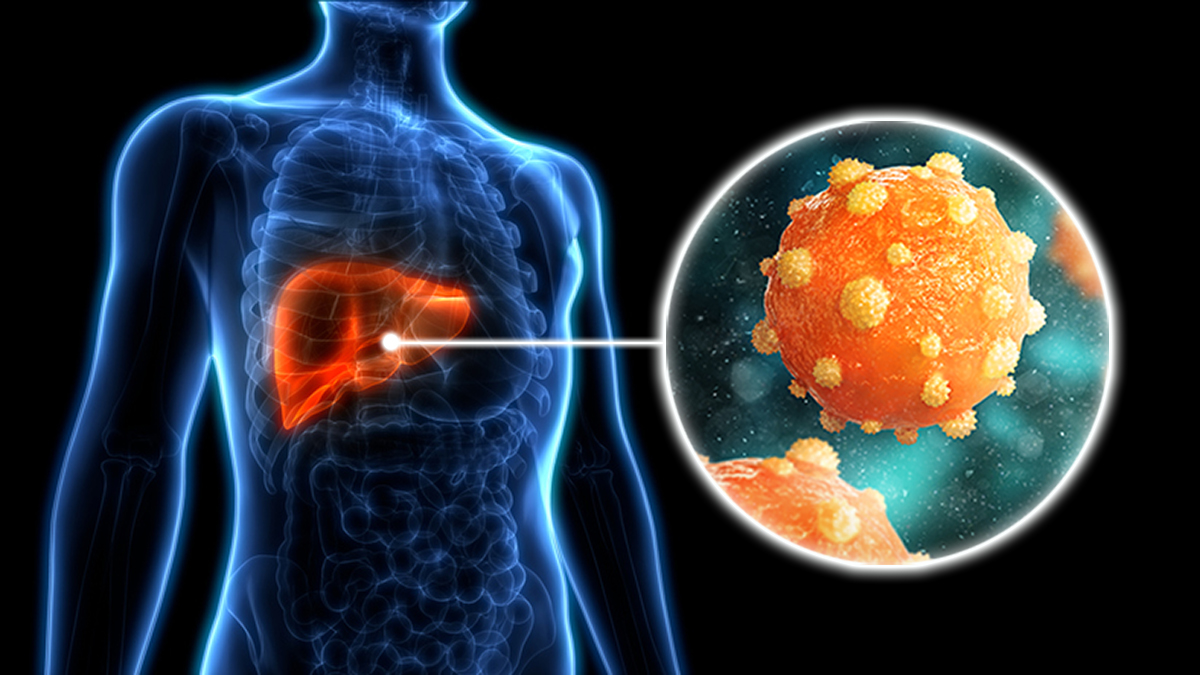
Hepatitis B is a life-threatening liver infection and is a serious healthcare issue. It is often transmitted via IV drug use, bodily fluids, spread from mother to child at birth, and sexual activity. The liver infection is caused by the hepatitis B virus (HBV) and can further damage the liver, resulting in acute hepatitis B or chronic hepatitis B, depending on how long the virus lasts for. If the disease continues for more than six months, it is chronic, which can put people at a high risk of death from cirrhosis, which is scarring of the liver, and liver cancer. Some symptoms include fatigue, nausea, dark urine, vomiting, and abdominal pain.
How?
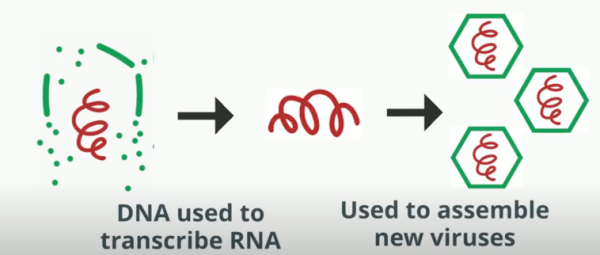
The HBV binds to a receptor on the surface of a hepatocyte. Upon entering the cell, the capsid or casing is disassembled, and the DNA inside is transported to the cell’s nucleus. HBV uses the hepatocyte’s machinery to make copies of itself by using its own DNA. Once all the required proteins and DNA are synthesized for a new virus, the HBV exits the hepatocyte to infect a new liver cell.
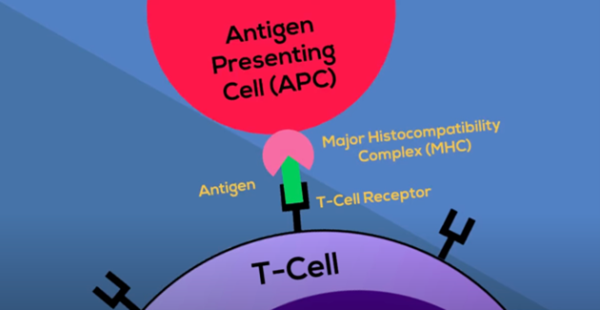
During the proliferation of HBV, the body’s immune system responds by attacking the cells that it thinks are infected. This is mainly a result of a cell-mediated adaptive immune response. It is called “cell-mediated” since it uses immune cells such as cytotoxic-T lymphocytes (CTLs) to kill HBV infected cells. T cells are activated when the T-cell receptor and a co-stimulatory molecule recognize an antigen on a complex called major histocompatibility complex (MHC). MHCs are on the surface of antigen-presenting cells (APCs); these cells recognize the virus as a threat and grind it up to prepare an antigen that the T cells can identify.
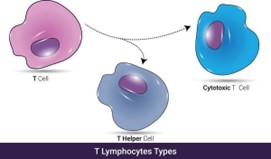 Afterwards, the T cell differentiates into T helper cells, which are responsible for producing cytokines that act as a signal for the development of CTLs. CTLs produce toxins that are similar to poison for the target cells. These toxic proteins can damage infected cells and make all their contents spill out, effectively killing the cells. When liver cells die in this fashion, it results in liver damage and the aforementioned symptoms seen in hepatitis B.
Afterwards, the T cell differentiates into T helper cells, which are responsible for producing cytokines that act as a signal for the development of CTLs. CTLs produce toxins that are similar to poison for the target cells. These toxic proteins can damage infected cells and make all their contents spill out, effectively killing the cells. When liver cells die in this fashion, it results in liver damage and the aforementioned symptoms seen in hepatitis B.
What Are CD8+ T Cells?
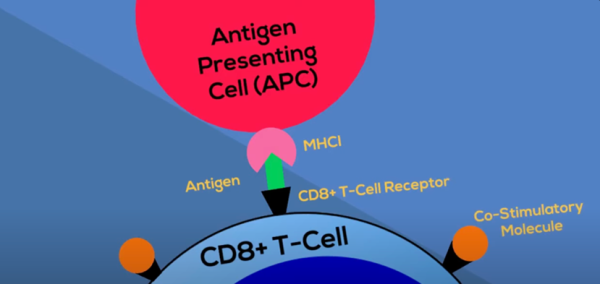
CD8+ T cells are major components of the cell-mediated adaptive immune response. Normally, they mediate protection against pathogens and tumor cells. In order to be activated, CD8+ T cells require two signals:
- Recognizing an antigen that is presented by MHC-1 complexes on APCs.
- Co-stimulatory signals provided by the same APC.
CD8+ T cells play a major role in controlling and resolving HBV infection. Emergex, a privately held biotechnology company, is in the process of developing a range of synthetic CD8+ T-cell priming immune set-point candidates designed to strengthen the body’s natural cellular immune response to destroy pathogen infected cells. Their mission is to provide an extra layer of immune protection for some of the world’s most infectious diseases. CD8+ T cells protect you by destroying harmful pathogens, which they do by sending signals throughout the body that help control the immune system’s response and threats.
While many organizations are researching for a treatment and cure for the world’s most impactful diseases, the Hepatitis B Foundation (established in 1991) promotes disease awareness and information for families and the scientific community with the collaboration of its two other organizations: the Baruch S. Blumberg Institute and the Pennsylvania Biotechnology Center. These three organizations are dedicated to upholding evidence-based scientific discoveries in a collaborative environment that prioritizes equity, respect, and inclusion of all community members. With the help of these kinds of organizations, diseases including hepatitis B and liver cancer can be treated more efficiently with advanced technology and medicine for future generations and for public health.